Mass casualty incidents do not care how prepared you feel. One moment you are running a routine call and the next you are surrounded by more patients than resources. This is where trauma triage and tagging becomes one of the most important skills in EMS.
Triage is not about being perfect. It is about doing the greatest good for the greatest number of patients with the information and tools you have in front of you. Whether you are an EMR on your first large scale incident or a seasoned paramedic renewing your certification, understanding how and why we triage matters.
This guide breaks down trauma triage and tagging using a practical, field focused approach built around the adult disaster triage image you provided. No fluff. No unnecessary jargon. Just the stuff you actually need when things get loud.
Why Trauma Triage and Tagging Matters in EMS
In single patient care, EMS is trained to do everything possible for that one person. In a mass casualty incident, that mindset must shift quickly.
Triage allows EMS to:
- Identify who needs immediate life saving care
- Allocate limited resources effectively
- Improve overall survival outcomes
- Maintain scene organization and provider safety
The emotional weight of triage is real. You may have to walk past someone who looks critically injured to help someone who has a better chance of survival. That does not make you heartless. It makes you effective.
The Foundation of Adult Disaster Triage Systems
Most EMS providers in the United States are taught the START triage system or a variation of it. START stands for Simple Triage and Rapid Treatment, and that name is not accidental.
Primary disaster triage focuses on three things:
- Ability to walk
- Respiratory status
- Perfusion and mental status
This initial sort should take less than 60 seconds per patient. If it feels rushed, that is because it is supposed to be.
Understanding the Four Triage Categories
The image you shared outlines the four core adult triage categories used in disaster medicine. Each color tag represents urgency, not value or worth.
Let’s break them down:
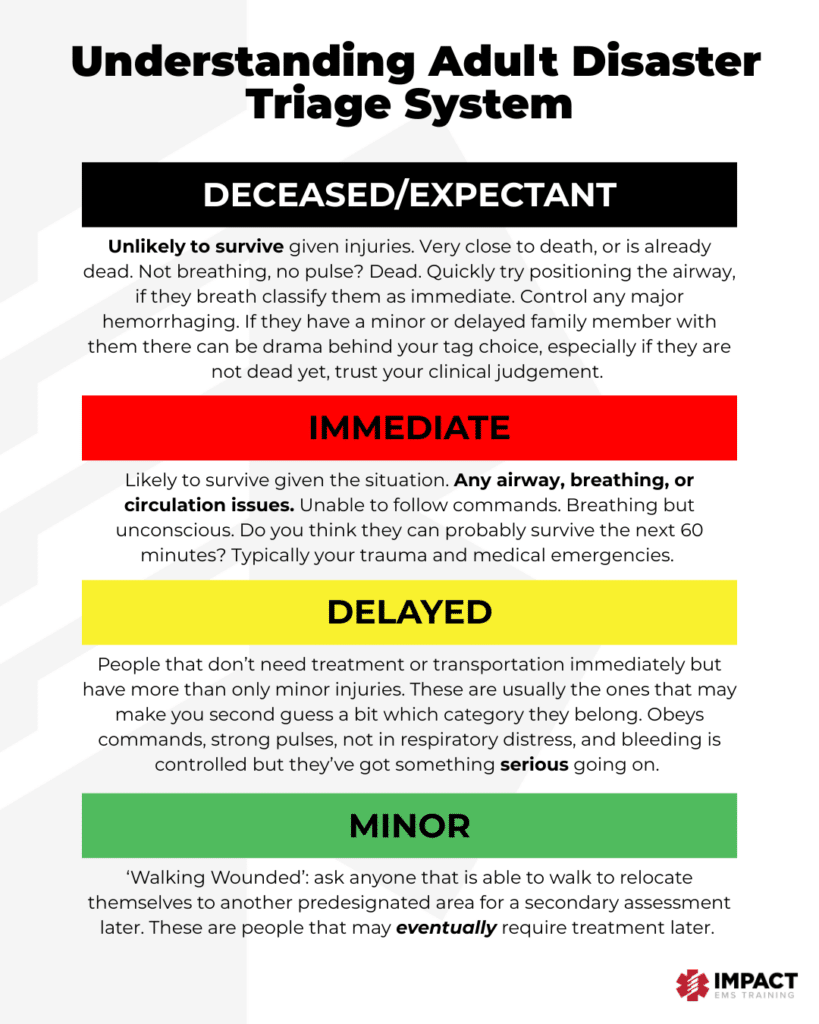
Deceased or Expectant: The Hardest Tag to Apply
This category is reserved for patients who are unlikely to survive given their injuries and the resources available.
Clinical indicators may include:
- Not breathing after airway repositioning
- No palpable pulse
- Injuries incompatible with life
One key point that often gets missed is airway repositioning. If a patient is not breathing, you should quickly open or reposition the airway. If they begin breathing, they are immediately reclassified as Immediate.
Emotionally, this category is tough. Family members may be present. Other providers may question your decision. This is where trusting your training and clinical judgment matters most.
Triage is not a declaration of death. It is a resource decision.
Immediate: Red Tags That Need You Now
Immediate patients are those who are likely to survive if they receive rapid intervention.
Common criteria include:
- Airway compromise
- Severe respiratory distress
- Uncontrolled hemorrhage
- Altered mental status or inability to follow commands
These are your classic trauma and medical emergencies that cannot wait. Think tension pneumothorax, severe bleeding, shock, or decreased level of consciousness.
If you are asking yourself whether they can survive the next 60 minutes without care, and the answer is no, they are probably red.
Delayed: Serious But Not First
Delayed patients have significant injuries but stable physiology for the moment.
Characteristics often include:
- Able to follow commands
- Adequate breathing
- Controlled bleeding
- Strong peripheral pulses
These patients make providers second guess themselves. They look bad, but they are not dying right now. Yellow tags require reassessment because patients can deteriorate quickly as the incident evolves.
Delayed does not mean unimportant. It means not first.
Minor: The Walking Wounded
Minor patients are often identified first by asking who can walk. Anyone who can ambulate is directed to a designated area for further evaluation.
Common features include:
- Minor lacerations
- Sprains or strains
- Emotional distress without physical injury
Green patients can overwhelm scenes if not managed well. Assigning a provider to oversee this group helps prevent secondary issues and keeps them from wandering back into the chaos.
Walking wounded still deserve care, just not immediately.
Practical Tips for Field Triage Success
Triage works best when it stays simple.
Helpful reminders:
- Do not overthink your initial triage
- Focus on physiology, not injury mechanism
- Re triage patients frequently
- Make tags visible and legible
Expect conditions to change. A yellow patient can become red. A green patient may reveal a hidden injury. Triage is dynamic.
Triage Errors That EMS Providers Commonly Make
Even experienced providers make triage mistakes, especially under stress.
Common errors include:
- Over triaging due to emotional pressure
- Under triaging because a patient is quiet
- Spending too much time on one patient
- Ignoring reassessment
Training helps reduce these errors, but awareness matters just as much.
Training for Triage Confidence and Competency
Triage is a perishable skill. Reading about it once in school is not enough.
High-quality EMS education should include:
- Scenario-based simulations
- Ethical discussion and debriefing
- Repetition across certification levels
- Real-world case reviews
Continuing education keeps these skills sharp and builds confidence before you need them.
Final Thoughts: Trust the System and Trust Yourself
Trauma triage and tagging is one of the most challenging responsibilities in EMS. It requires speed, confidence, and the ability to make decisions under pressure.
The system works when providers trust it. Your job is not to save everyone. Your job is to save as many as possible.
And yes, you are allowed to feel weird about it afterward. That part means you care.