If you’ve ever stared at a monitor, wondering what those squiggly lines look like and if what you’re seeing is a normal or a bad rhythm, this post is for you!
You don’t need to be a paramedic to recognize a life-threatening cardiac rhythm. Today’s EMTs are increasingly expected to place 12-lead cables, assist with cardiac arrest care, and most importantly, know what you might be looking at.
Let’s break down the four most dangerous rhythms you’ll encounter in EMS – and how to respond with confidence, not guesswork.
Why Rhythm Recognition Matters for EMTs
While EMTs aren’t typically responsible for full ECG interpretation, many operate cardiac monitors, assist with defibrillation, and perform high-quality CPR as part of an EMS team. In some states and agencies, EMTs are trained to identify shockable rhythms and initiate early defibrillation, even without ALS on scene.
Knowing what you’re looking at can save time, improve patient outcomes, and support your ALS team in real emergencies.
Ventricular Fibrillation (V-Fib)
What It Looks Like:
Chaotic, disorganized squiggly waves on the monitor. No identifiable P, QRS, or T waves. It looks like a mess, and it is a hot mess.
What It Means:
The heart’s electrical system has gone haywire. The ventricles are quivering, not contracting, which means no cardiac output and no perfusion to vital organs.
Causes:
- Acute myocardial infarction
- Severe electrolyte imbalance
- Drug toxicity
- Hypoxia
- Trauma or structural heart damage
EMS Response:
This is a shockable rhythm. Immediate defibrillation + high-quality CPR are your best tools. Each minute without defibrillation decreases survival by 7-10%.
Think of it like a “reset button” for the heart, just like law enforcement uses a taser to stop chaotic behavior and restore control.
Ventricular Tachycardia (V-Tach)
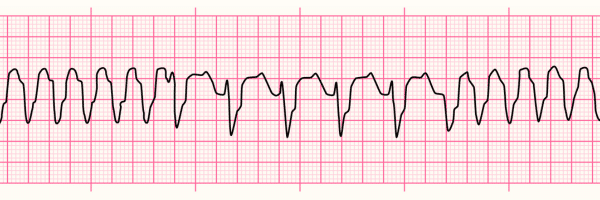
What It Looks Like:
Fast, wide QRS complexes can be regular (monomorphic) or irregular (polymorphic, like torsades de pointes).
What It Means:
The ventricles are firing too rapidly to allow effective filling and ejection. This may lead to low perfusion or cardiac arrest.
Perfusing vs. Pulseless:
- With a pulse: Patient may be alert but symptomatic (dizzy, chest pain, hypotensive).
- Without a pulse: Treat as a cardiac arrest with immediate CPR and defibrillation.
Causes:
- Structural heart disease
- Scar tissue from MI
- Medications or drug toxicity
- Electrolyte abnormalities (especially potassium and magnesium)
EMS Response:
- Pulseless V-Tach: Defibrillate immediately.
- With a pulse: Prepare for cardioversion; notify ALS if you’re BLS.
“Monomorphic means one direction. Polymorphic? Multiple. Both can kill if not treated fast.”
Pulseless Electrical Activity (PEA)
What It Looks Like:
A strip that looks normal (or almost normal) but the patient has no pulse.
What It Means:
There is electrical activity, but the heart is not mechanically contracting, or it’s contracting without generating perfusion. This is a pump (heart) problem, not an electrical one.
“Think of it like a fire pump with no water. The engine’s running, but nothing’s flowing.”
Common Causes (6 Hs and 6 Ts):
- H: Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hypo-/Hyperkalemia, Hypothermia, Hypoglycemia
- T: Toxins, Tamponade, Tension pneumothorax, Thrombosis (coronary or pulmonary), Trauma
EMS Response:
Start CPR immediately. Do not defibrillate! PEA is not a shockable rhythm. Address reversible causes if known.
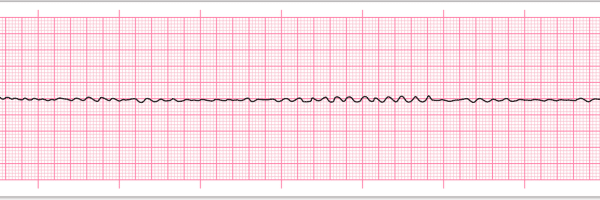
Asystole
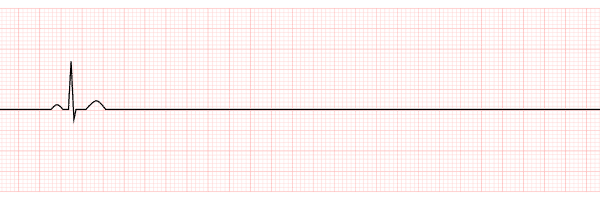
What It Looks Like:
The flat line. No electrical activity at all.
What It Means:
There’s no electrical impulse in the heart, no activity to restart. This is often the final stage after an untreated arrest or prolonged hypoxia.
Movie Myth:
TV loves to show people getting shocked back to life from a flatline. That’s fiction.
EMS Response:
- Start CPR
- Do not defibrillate
- Continue resuscitation per protocol (likely ALS-dependent)
Field Tips for Rhythm Recognition
- Always check a pulse. What you see on the screen means nothing without a pulse check.
- Practice reading real strips. There’s no shortcut! Build familiarity with training and case studies.
- Use mnemonics and checklists. Remember shockable vs. non-shockable, and use protocols like a script under pressure.
Extra Tips
- Defibrillation within the first 3 minutes of cardiac arrest improves survival by up to 74%.
- PEA can present with a normal-looking strip. Always check a pulse.
- Asystole has the lowest survival rate of all cardiac rhythms. Remember: it is not shockable.